It’s time for Dental for All
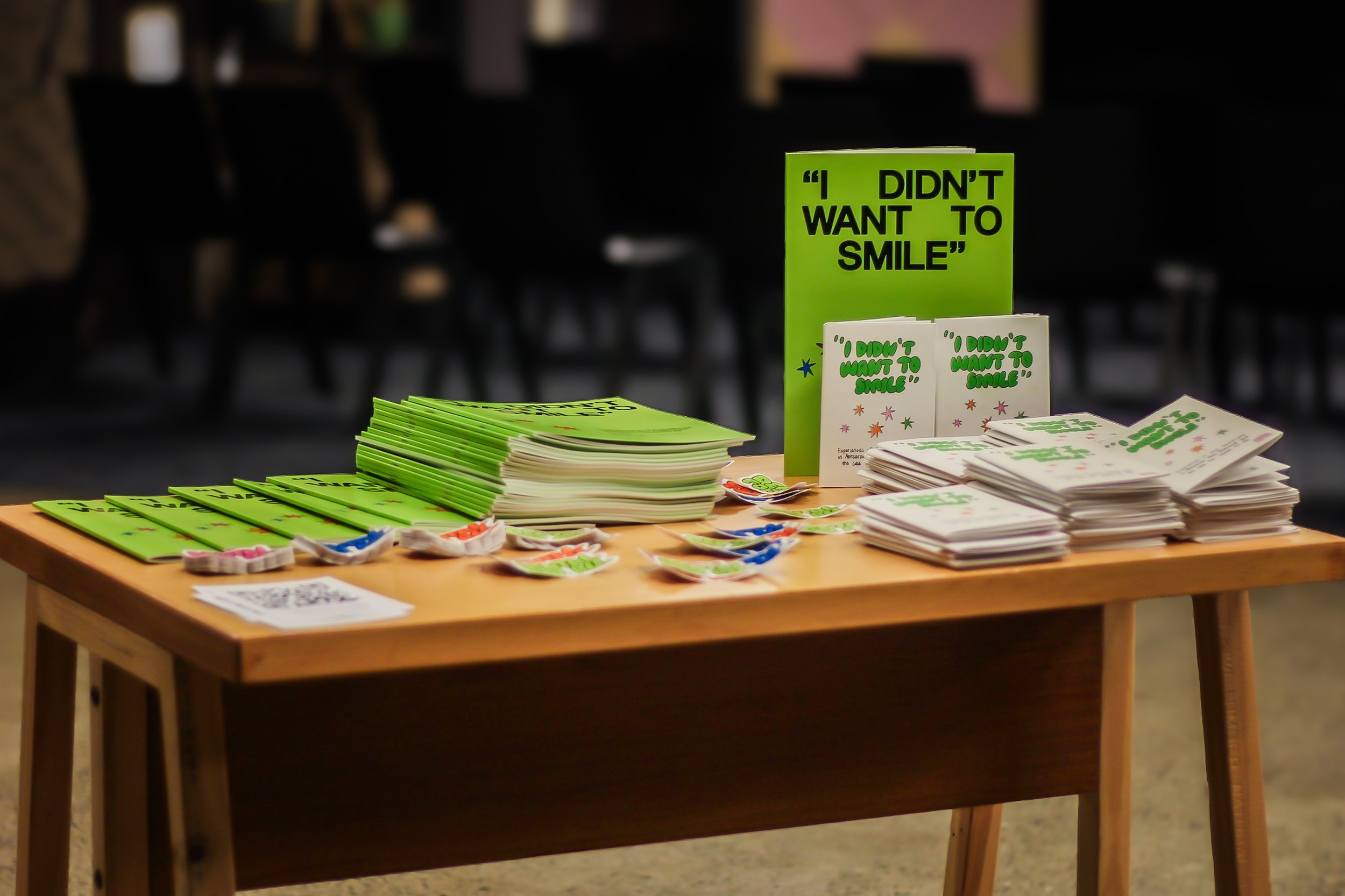
It’s been about 6 weeks since my latest report “I Didn’t Want to Smile: Experiences of Oral Healthcare in Aotearoa New Zealand and the Case for Dental for All” was released. I’ve taken some time to write up some of the core themes and what the research felt like below.
Does this report resonate with you? Do you have some reckons you want to share? Get in touch: kayli.taylor.public@gmail.com
The report
Over 2024, I spoke to 10 people from across Aotearoa New Zealand about their experiences of accessing dental care in our current system. These 10 stories were written up in a report that was published in February 2025. The report includes the stories (written up as first-person narratives with pseudonyms) and thematic analysis of the issues surrounding access to dental care in Aotearoa. The report didn’t set out to be representative of every person’s experiences of oral healthcare in Aotearoa, or provide solutions to the complex issues presented. It does however, share 10 very different stories of struggle and shame in relation to accessing oral healthcare. The clear theme across the stories is that the status quo is not working. We need change.
I encourage everyone to read the stories in this report and take the time to sit with them. The report was also covered in the media. On the Herald, Newstalk ZB, and PMN, TVNZ Breakfast, RNZ, and the Kākā podcast with Bernard Hickey.
What story-sharers said
The people I spoke to shared painful experiences of New Zealand’s current oral healthcare approach. Cost was identified by story-sharers as the major factor that stopped them from accessing the oral healthcare they needed. Data from the most recent New Zealand Health Survey shows that nearly half (44.9%) of adults reported unmet need for dental care due to cost. These rates were higher for Māori (54.1%), Pasifika (57.2%), those with disabilities (53.2%), and those aged 25-34 (57.2%). We know that the high costs of dental care are preventing us from accessing the oral healthcare we need.
These high costs force people to make hard or impossible choices – such as going into debt to afford dental care, delaying their treatment, not doing the treatment, and choosing dental care over other forms of healthcare (such as visits to the optometrist). Several people to shared their stories with me said they had relied on GPs or other aspects of the health system, because they could not afford the dentist. This included treating GPs as a first port of call when their teeth went a bit translucent or to get antibiotics for an infection.
Reflecting on the research process
The research process was long. From the beginning of the project, I embedded processes that allowed to it to be as story-sharer led as possible. They checked their story summaries, then the text of their stories, then the illustrations that accompanied their stories. Huge mihi to MIL HAMPY for the amazing illustration work & Anastasia Burn for their design work. The process contained lots of grief for me. In conversations both face to face and online, I felt some of the mamae (hurt) that story-sharers felt: the stigma they experienced in trying to access dental care. Engaging with empathy is essential to research, particularly interview-based research. It was a huge privilege to listen to these stories, grieve, and dream with these brave story-sharers.
I felt an embodied response to some of the stories shared. During and after interviews and conversations, I could feel emotions bristling in me – frustrations at our high-cost, exclusionary dental system; grief at the experiences people had; and a passion to continue this essential research and advocacy. Long, fast walks were essential to my wellbeing – being outside in fresh air and letting my energies go through physical exercise. As were conversations with those who got it – huge thanks to Max and Hana, my colleagues at ActionStation, for helping channel my frustrations into action.
Where to from here?
We know the current oral healthcare system is not fit for purpose. The high cost is preventing people from accessing the care they need – with huge consequences on their emotional and physical wellbeing. We know that good oral healthcare is essential to the wellbeing of people and communities. We also know that the social, economic, and fiscal costs of oral healthcare in New Zealand (estimated between $5 billion and $11 billion per annum) far exceed estimates for what it would cost to fund to fund free and universal oral healthcare (likely $1.5 billion per annum). Based on this research, I believe it is essential we implement free and universal oral healthcare for all. Several story-sharers said that this would be “life-changing”. That new oral healthcare framework must centre te Tiriti o Waitangi – the foundational document of Aotearoa New Zealand that gives us all a vision of a better future.
The Dental for All team is hitting the road in August – October 2025, sharing this report and our other mahi across the motu. We are hoping to chat to folk from across Aotearoa New Zealand about their experiences of oral healthcare and show you that a better world is possible where everyone in Aotearoa has access the oral healthcare we all need and deserve. If you’d like us to visit you and your community, please reach out: kayli.taylor.public@gmail.com